Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
From gut bacteria gone rogue to life-threatening heart disease — researchers reveal how tweaking your microbiome could be the next frontier in preventing cardiovascular problems.
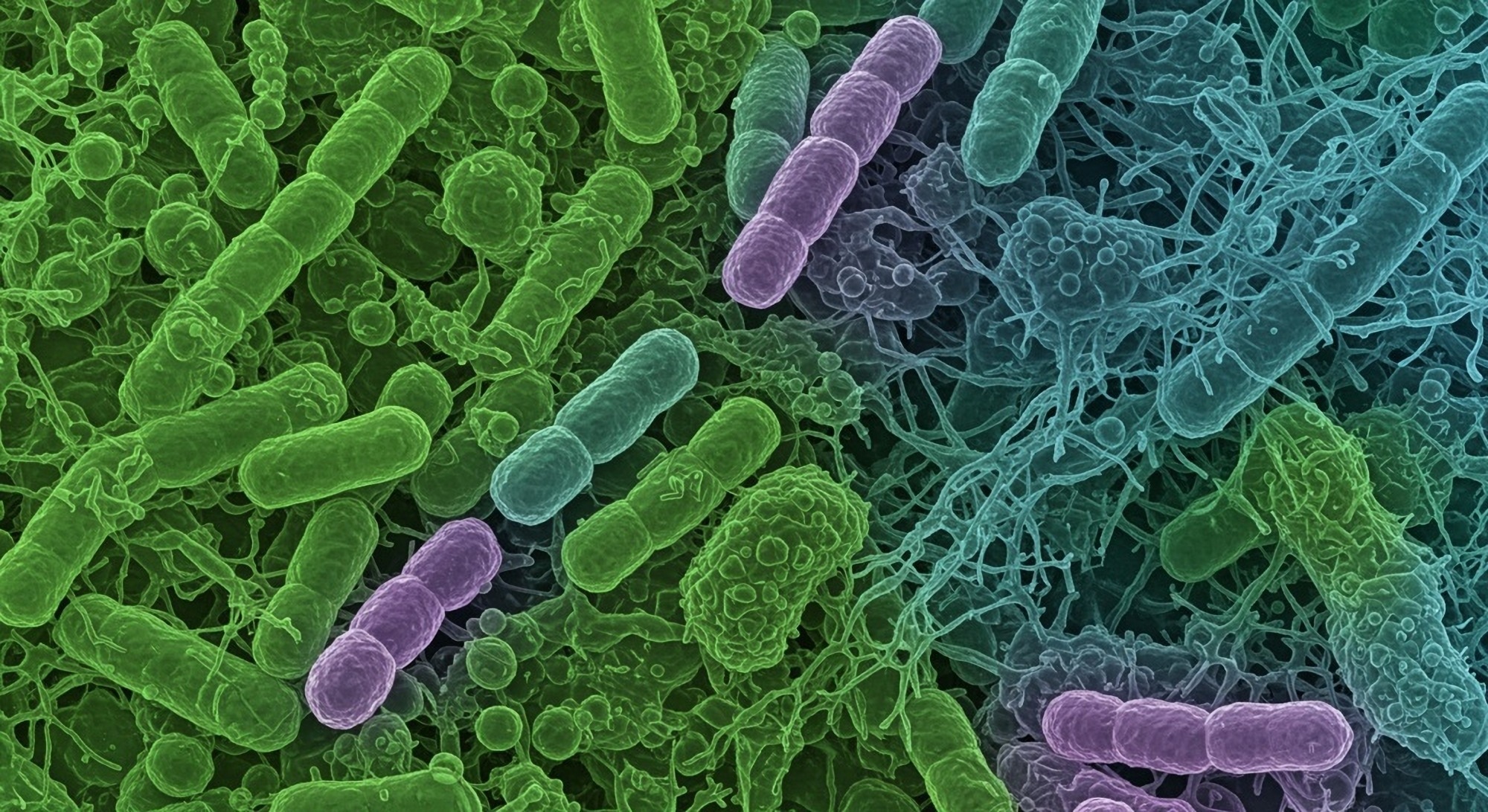
 Study: Beyond the Gut: Unraveling the Multifaceted Influence of Microbiome on Cardiovascular Health. Image Credit: Shutterstock AI Generator / Shutterstock.com
Study: Beyond the Gut: Unraveling the Multifaceted Influence of Microbiome on Cardiovascular Health. Image Credit: Shutterstock AI Generator / Shutterstock.com
In a recent study published in Clinical Nutrition ESPEN, researchers review the role of the gut microbiome in maintaining cardiovascular health.
Cardiovascular disease (CVD) is a leading cause of mortality worldwide. A previous diagnosis of diabetes, hypertension, or dyslipidemia, certain medications, and lifestyle factors like smoking, drinking, poor diet quality, and lack of exercise may increase the risk of developing CVD.
Chronic kidney disease is also widely prevalent throughout the world, with about 10% of individuals currently diagnosed with this disease. Chronic kidney disease varies in severity, with some individuals retaining their kidney function despite damage to end-stage renal disease. Like CVD, the risk of chronic kidney disease also rises in the presence of obesity, diabetes, and hypertension.
Hypertension is a significant risk factor for both chronic kidney disease and CVDs. Salt consumption is the most common environmental factor that increases leads to hypertension.
Salt, otherwise known as sodium chloride, is an ionic compound primarily absorbed by the intestinal mucosa. Consuming foods high in salt can lead to microvascular endothelial inflammation, morphological remodeling, and functional issues.
Certain segments of the population are particularly sensitive to the effects of salt, as their blood pressure levels can change in response to salt intake, while other individuals may not be unaffected by these foods. Salt sensitivity can arise due to genetic polymorphisms of the renin-angiotensin-aldosterone system (RAAS), dietary intake, or the presence of kidney disease.
SCFAs
Short-chain fatty acids (SCFAs) produced by gut microbiota regulate blood pressure by interacting with various receptors, including G protein-coupled receptors like GPR41, GPR43, and olfactory GPR78 (Olfr78). Activation of these receptors leads to the production of nitric oxide (NO) and regulation of RAAS, both of which cause vasodilation.
Acetate, propionate, and butyrate account for 60%, 20%, and 20% of the gut microbiome’s total SCFA production, respectively. However, alterations in the gut microbiome’s composition can reduce SCFA production, thereby increasing the likelihood of a hypertensive state.
Previous studies using rodent hypertension models have reported that SCFAs are crucial for maintaining the integrity of the intestinal barrier through their anti-inflammatory effects on both colonic epithelium and immune cells. For example, butyrate stabilizes hypoxia-inducible factor-1 (HIF-1), which reduces blood pressure levels and further preserves the functionality of the intestinal barrier by reducing its permeability.
TMAO
High circulating levels of the gut metabolite trimethylamine n-oxide (TMAO) can lead to aortic stiffening, thereby increasing systolic blood pressure levels and the risk of CVDs. High-fat foods like red meat, milk, and fish are often rich in phosphatidylcholine, choline, and l-carnitine, all of which are precursor molecules to trimethylamine (TMA) and TMAO.
High plasma levels of TMAO can also arise due to increased salt intake, which may lead to atherosclerosis, non-fatal myocardial infections, hypertension, and stroke. Recent animal studies have reported that experimental suppression of flavin-containing monooxygenase 3 (FMO3), an enzyme involved in TMAO synthesis, leads to a significant reduction in atherosclerotic plaque formation and an improvement in cholesterol metabolism.
The release of TMAO into systemic circulation can also lead to the oxidation of low-density lipoproteins (LDL), which can prevent efficient vasodilation. High levels of oxidized LDL cholesterol can lead to excess endothelin-1 production, which causes vasoconstriction and hypertension.
TMAO is also considered a pro-inflammatory substance, as its release induces the production of reactive oxygen species (ROS) and pro-inflammatory cytokines, both of which lead to vascular inflammation and endothelial dysfunction.
Lipopolysaccharide
Lipopolysaccharide (LPS) is produced during gut dysbiosis, which arises due to an imbalance in the ratio of pathogenic to beneficial bacteria in the gut microbiome. Once released into the systemic circulation, LPS can induce inflammation by binding to Toll-like receptor 4 (TLR4), which can lead to the production of pro-inflammatory cytokines like interleukin 6 (IL-6), IL-1, IL-27, and tumor-necrosis factorα.
The use of prebiotics, probiotics, and dietary modifications aimed at re-establishing a balanced gut microbiota can boost SCFA production and decrease TMAO levels.”
Prebiotics, which promote the growth of beneficial bacteria in the gut, and probiotics, which deliver beneficial bacteria to the gut, have been investigated for their potential to achieve homeostasis in the gut microbiome and promote cardiovascular health. However, additional studies are needed to determine the effectiveness of these treatments, as published studies have reported mixed results.
A balanced diet, sufficient physical activity, and stress management are key to maintaining a healthy gut microbiome. Thus, interventions that facilitate these lifestyles can be effective in reducing the risk of CVDs.
Fecal microbiota transplantation involves transferring fecal matter from a healthy donor to a patient and has shown promising outcomes in treating gut-related conditions. This intervention may also have potential application in the context of cardiovascular diseases.
Journal reference: